PCS Clinical Competencies for RNs
PULSELSS ALGORHYHM
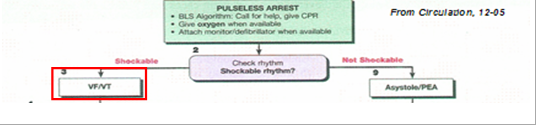
The 2005 Guidelines have combined all pulseless algorithms into one decision tree. As with the BLS standards the emphasis is on providing consistent high quality compressions.
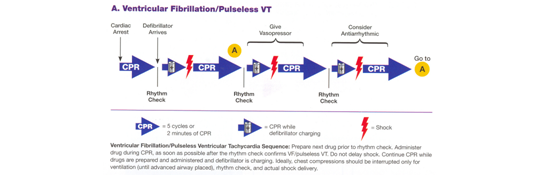
If the rhythm is ventricular fibrillation (VF) or pulseless ventricular tachycardia(VT):
DEFIBRILLATION Witnessed v. Unwitnessed Arrests 2005 GUIDELINES: It the arrest is unwitnessed and the exact time the patient has been down is unknown, perform 2 minutes of CPR prior to evaluating the cardiac rhythm with an AED. If the arrest was witnessed, attach the defibrillator as soon as possible and evaluate the cardiac rhythm for potential defibrillation. 2000 GUIDELINES: Attach the defibrillator and evaluate the rhythm as soon as the unit is available. WHY THE CHANGE? Research suggests that patients who do not have a pulse for periods of longer than four minutes are less likely to respond to defibrillation. Two minutes of CPR appears to make the heart more likely to respond to defibrillation.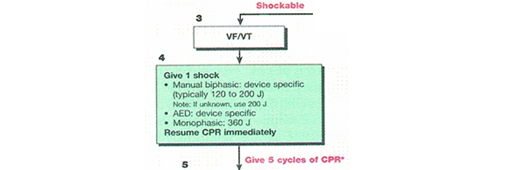
Number of Shocks 2005 GUIDELINES: One shock followed by immediate CPR for two minutes prior to pulse check or rhythm evaluation. Recommended energy levels for monophasic defibrillators (e.g. the LifePack 9Ps on most crash carts, or the LP10s on some units) should start at 360 Joules. NOTE: the energy level must be manually adjusted by the operator. Biphasic defibrillators should start at 200 Joules. Currently biphasic defibrillators are stocked on CICU, 3E, OR, MIPS and the Echo Lab. 2000 GUIDELINES: Up to three stacked shocks with rhythm evaluation between each defibrillation. |
WHY THE CHANGE? Researchers who have examined the efficacy of defibrillation found that the majority of people, who will respond, will do so after one shock. Very few will respond to the second or third shock. Repeated rhythm evaluations can lead to long interruption in compressions. Additionally, if a patient does develop a pulse after being defibrillated, the majority will convert to a non-perfusing rhythm (e.g. pulseless electrical activity) for several minutes after their heart starts beating in an organized rhythm. They seem to benefit from the ongoing compressions. |
VASOPRESSOR THERAPY
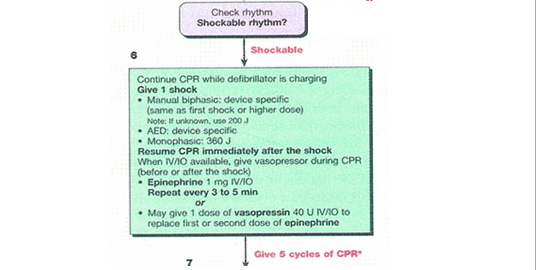
2005 GUIDELINES: If the patient continues in to have a shockable rhythm after the two minutes of CPR consider administering epinephrine 1 mg IV/IO or vasopressin 40U IV/IO for the first or second dose of epinephrine. 2000 Guidelines: Vasopressin could only be substituted for the first dose of epinephrine. WHY THE CHANGE? The research supports the safety of vasopressin; however current recommendations are to give it only at the beginning of the code. There is no data to support giving it any more frequently. A BRIEF WORD ABOUT THE IV/IO The AHA has found that if IV access cannot be obtained, intraosseus (IO) is the preferred route in adults over the endotracheal route. This is primarily a field recommendation, and HAS NOT BEEN APPROVED FOR USE AT HMC AS OF THIS DATE. We will continue to evaluate this on a continuing basis, so stay tuned. ANTIARRYTHMIC THERAPY
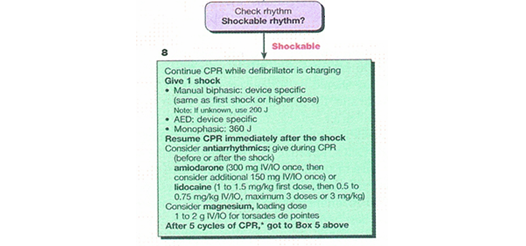
2000 GUIDELINES: Included procainimide. WHY THE CHANGE? Amiodarone is still the antiarrythmic agent of choice if it is available. |
Continue to cycle through the algorhythm as long as the rhythm remains VF or pulseless VT. |
ASYSTOLE and PEA
Many of the causes of asystole and pulseless electrical activity (PEA) are similar to the other pulseless rhythms. The new combined guidelines reinforce the rapid assessment of potential etiologies. This is summarized as the so-called "Hs and Ts". H's - Hypovolemia - Hypoxia - Hydrogen ions (acidosis) - Hypo / hyperkalemia - Hypoglycemia - Hypothermia T's - Toxins (overdose) - Tamponade, cardiac - Tension pneumothorax - Thrombosis (coronary or pulmonary) - Trauma
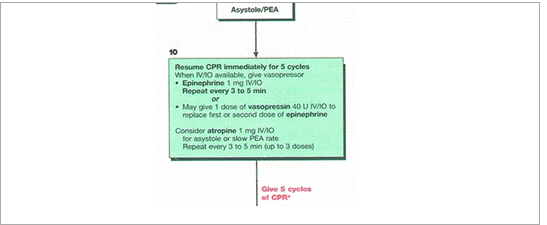
2005 GUIDELINES: Epinephrine 1mg IV/IO repeat every 3-5 minutes OR Vasopressin 40 Units IV/IO to replace the first or second dose of epinephrine. Atropine 1 mg IV/IO for asystole or slow PEA rate repeats every 3-5 minutes up to 3 doses. Transcutaneous pacing (TCP) is not longer recommended for use in asystole. 2000 Guidelines: Included epinephrine and atropine 1 mg IV for asystole or slow PEA rate. TCP was an option early in the treatment of asystole. WHY THE CHANGE? Vasopressin appears to be a viable in converting PEA and asystole. However, no efficacy over epinephrine was found. Use of TCP in asystole did not show a return of circulation or an improvement in outcome. |
POST RESUSCITATION CARE 2005 GUIDELINES: Continue with 5 cycles of compressions, approximately 2 minutes after the return of an organized rhythm. Other interventions such as fluid administration, anti0arrythmic therapy, vasopressor or inotropic therapy should still be considered. WHY THE CHANGE? The majority of research found that the majority of patients return to a non-perfusing rhythm. The additional compressions may assist in improving mortality. 2000 GUIDELINES: General interventions such as fluid administration, anti0arrythmic therapy, vasopressor or inotropic therapy should still be considered. |
BRADYCARDIA AND TACHYCARDIA
Both of these algorhythms have undergone reformatting and streamlining for clarity. However there are minimal content changes.
Last modified: 5/24/2006 8:36 AM